Report
By the
Budget Committee
On the
2003 Budget
With Recommendations
![]()
Adopted by
AMHB Budget Committee –
Adopted by
AMHB –
Report
By the
Budget Committee
On the
2003 Budget
And Recommendations
June, 2003
Report
By the
Budget Committee
On the
2003 Budget
With Recommendations
![]()
Adopted by
AMHB Budget Committee –
Adopted by
AMHB –
Report
By the
Budget Committee
On the
2003 Budget
And Recommendations
June, 2003
VII. Evaluation
of The Budget Building Process
A. Funding Should Be More
Explicitly Tied to Desired Results
B. Medicaid/SSDI/SSI
Should Be Re-Tooled as Possible to Achieve Desired Results
D. The Budget Building
Process Should be Re-evaluated.
The
focus of the Alaska Mental Health Board's 2003 Budget Summit was to look at
what is being "purchased" by the Mental Health Program (Program) and,
if it is not what is desired, make recommendations regarding how to make it do
so.
•
Funding should be based on achieving desired
results and those should be achieving the goals of consumers.
•
In order to achieve this, the Mental Health
System (System) should be flexible and needs based.
•
The System should if at all possible respond
before a person is in crisis.
•
Medicaid, Social Security Disability Income
(SSDI) and Supplemental Security Income (SSI) should allow or, better yet,
facilitate people returning to the mainstream, including gainful employment in
appropriate jobs.
There
were discussions of what data the System should be collecting and using to
evaluate and manage the Program as well as whether it was clear enough from the
data that the current reliance on psychiatric medications substantially
increases chronicity. These and similar
items are referred to the full Board/Planning Committee for further development
and consideration.
The
Budget Summit was "kicked off" on
The
Budget Summit continued in Anchorage on April 11-12, 2003, with all 4 Budget
Committee members present (Jim Gottstein, Tony Mander, Barry Creighton, Keggie
Tubbs), 3 other Board Members attending, Jeanette Grasto, Tracy Barbee and Bill
Hogan, staff Kate Webster and Kay Klose, 3 other Division of Mental Health and
Developmental Disabilities (DMHDD) personnel, and 5 or so other people
representing stakeholders and the public in attendance all or part of the
time. April 11th was devoted to
presentations of information, including updated budget and outcome data, public
input, and a roundtable discussion over what should be in the final report and
recommendations. On April 12th, the
discussion of recommendations and conclusions continued. This Report was unanimously adopted in
concept on
(a) The
[Trust] shall annually, not later than September 15, submit to the governor and
the Legislative Budget and Audit Committee a budget for the next fiscal year
and a proposed plan of implementation based on the integrated comprehensive
mental health program plan prepared under AS 47.30.660(a)(1). The budget must
include the authority's determination of the amount
(1)
recommended for expenditure from the general fund during the next fiscal year
to meet the operating and capital expenses of the integrated comprehensive
mental health program;
(2) in
the mental health trust settlement income account, if any, that is not
reasonably necessary to meet the projected operating and capital expenses of
the integrated comprehensive mental health program that may be transferred into
the general fund; and
(3) of
the expenditures the authority intends to make under AS 37.14.041 and
37.14.045, including the specific purposes and amounts of any grants or
contracts as part of the state's integrated comprehensive mental health
program.
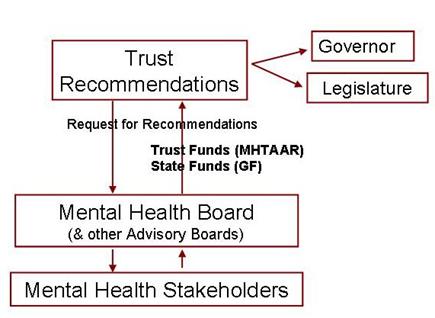
Under
AS 37.14.045 and the Settlement Agreement, the Trust has the power to spend
Trust Fund income (MHTAAR)[2] directly
without an appropriation; however state agencies need an appropriation to spend
the funds. In order for the Trust to
develop its budget recommendations, it requests recommendations from the four
Trust beneficiary boards[3] (Request
for Recommendations or RFR).
The
Trust explains the process this way:
The
Separate Appropriation Bill
The separate appropriations bill for the
Comprehensive Integrated Mental Health Program includes several components.
They are:
General
Fund/Mental Health Base (GF/MH Base): This is the amount
established by identifying the mental health services funded within the state's
general fund budget. The Trustees calculated that amount to be $131 million for
fiscal year 2003. These general funds are designated as general fund/mental
health dollars, or GF/MH Base. The final budget from the previous fiscal year
establishes the GF/MH Base.
Adjustments
to the Base: As The Trust and the associated boards and commission
further refine the definition of beneficiaries and accurately track funds for
the Comprehensive Integrated Mental Health Program, the Trustees suggest
adjustments to the base each year.
GF/MH
Increments: When the Trustees identify better and more cost
efficient ways of providing on-going services or providing for unmet needs,
they make recommendations in the form of GF/MH increments.
Capital
Budget: The separate appropriations bill includes that portion
of the state’s capital budget that funds mental health projects. This often
includes funds from the Alaska Housing Finance Corporation to provide housing
for beneficiaries as part of the Comprehensive Integrated Mental Health
Program.
Mental
Health Trust Authority Authorized Receipts (MHTAAR): The
Trustees authorize state agencies to spend Trust funds for specific operating
and capital projects. These state agencies must have legislative approval to
receive and expend Trust funds.
The
Trustee’s recommendations for the mental health bill are due to the governor on
September 15th for the following state fiscal year. However, because the
Trustees rely heavily on the recommendations of the four Advisory Boards, the
Trust budget process actually begins early in the calendar year when the Trust
sends the Advisory Boards a Request for Recommendations (RFR). The Trustees
review these recommendations in late summer and make their funding decisions in
time to meet the September 15th deadline.
The
Board also seeks input from its stakeholders in the Request for Recommendations
process and many stakeholders identify mental health service needs that they
would like to have funded. The Board
takes this information and then makes decisions on what to recommend to the
Trust. In doing so, the Board does not
normally recommend that any particular program get funding; rather it takes
specific proposals that it receives and converts them into a
"generic" budget category.
The following graphic illustrates this budget building process:
It is
not possible at this juncture to say what the total mental health budget is
because it is spread across so many different budget categories and agencies.
No one has attempted to compile such a total since the early 1990's when it was
done in connection with the Mental Health Trust Lands Litigation. In addition
there is not agreement as to what expenditures should be included as being part
of the Mental Health Program. What could
be identified follow:
As can
be seen from the below figures expenditures for inpatient services is very
close to that spent on Community Mental Health.
Also, Medicaid paid $19
Million for psychiatric drugs in FY 02.
Another comparison raising questions is the per capita and per client
range of Community Mental Health Grant and Medicaid Expenditures:[4]
While
it is clear there are great disparities in per capita and per client
expenditures between community mental health centers it is important to be
careful in drawing conclusions because of various factors. For instance, there is a high probability
that high needs clients migrate to the larger cities where more intensive
(costly) services are provided and that community mental health centers with
small catchment populations can not spread their overhead across as many
people. Having said that, however, there
are still great differences that suggest widely varying Medicaid billing
practices and possible over reliance on grant based services.
As to
where Community Mental Health dollars are going, the available data revealed:
At the end of the "Kick-Off" in March, the following question was posed. Is the Budget Purchasing?
| Housing Relationships Jobs/Meaning In life Recovery |
|
Protection |
The system increasingly talks
about the items on the left as being the desired results, but with the possible
exception of "dependency" the other results have also been seen as
desirable. In fact,
"protection" and "control" have been suggested as the
primary reason that the public pays for mental health services. Protection includes the community as well as
the recipient and is clearly a highly valued result. While perhaps not viewed as positively,
controlling disturbed and disturbing behavior has also been a major goal of the
public mental health system.
Stabilization is a good outcome when compared with deterioration and
also if the course of mental illness is assumed to be a steady or progressive
worsening of condition. However, good
housing, relationships, being productive and recovery are all preferred and, to
the extent they are achieved, the other goals no longer need to be achieved.
It is
being accepted around the country that recovery from mental illness is possible
for many people that have previously been considered to be destined to a life
of great disability. The most important
factors identified in recovery are Hope, Housing, Relationships, and
Employment/Meaningful Activity. As the
focus of the program shifts towards improvement in the lives of mental health
system recipients the question arises whether we are purchasing these
results. There is even more limited data
regarding these results.
Data
from the Division of Mental Health and Developmental Disabilities' Management
Information System on housing status indicates that 29 % of community mental
health center clients live either alone or with an unrelated person(s) and 54%
live with a relative(s) (54%). The
remaining 17% are shown as "Housing Unknown." It does not seem safe to assume that all of
the unknown are homeless, nor is there great confidence that the other
categories exclude being homeless. The
Mental Health Board, as part of its planning process, has estimated there are
approximately 1,400 of its beneficiaries who are homeless. Another factor that is not addressed is
whether consumers consider their current housing situation ‘ideal’ or whether
they even consider it safe and affordable.
One area that there is some data on is employment:
·
Only 1% of
·
Less than 1% of people go from SSDI to Employment
·
Less than 10% of people on SSI are gainfully
employed.
This data starkly shows that
under the present system once a person gets placed on SSDI they are very
unlikely to ever return to the workforce.
Since placement on SSDI and SSI are criterion for receiving Medicaid
services, and that people have to be both disabled and very poor to be in these
programs, the clear result of this funding mechanism is that the Medicaid/SSDI/SSI eligibility and
funding mechanism is essentially a one way ticket to permanent disability and
poverty. This is probably the single most important
information contained in this report.
The
Trust was extraordinarily successful in leveraging its relatively small
financial contributions to the mental health program to not only prevent budget
declines, but increase the mental health program budget during a time of budget
declines. It was able to do this at
least in part through the process outlined above by recommending
"increments" (increases) and using Trust Funds to get programs going
and then moving them to other funding sources, which was typically the General
Fund.[5] The value of being able to bring even the
relatively small amount (but in the millions of dollars) it has "to the
table" is much more than the amount it has to contribute and the Trust has
been incredibly skillful in this process.
However, due to the financial crisis the state is facing, it appears
that for the first time this strategy was unsuccessful and Program funding is
faced with a substantial General Fund decline.
All
processes should be periodically reviewed to determine if they continue to
optimize results. The state's budget
crisis, the new administration resolved to reduce spending to address this
crisis, the increasing reliance on federal funds (e.g., Medicaid) and data
results suggests this is a good time to re-evaluate
A
number of things leap out from the circumstances and data. The first is the absence of consideration of
Medicaid mental health expenditures in the budget building process, which
equals or exceeds the parts of the budget that is part of the Trust's Request
for Recommendation process. The second
is that the focus on increments (increases) may no longer be tenable. Perhaps even more important is by not looking
at the effectiveness of expenditures in the "base" (which this Report
suggests should include Medicaid) in achieving desired Results, there has been
little, if any incentive or requirement to achieve desired Results. In other words, the entire mental health
budget program should be evaluated.
Therefore,
it is suggested that the Board should regularly and rigorously review results
and identify gaps, rather than relying so heavily on stakeholders bringing
specific proposals for consideration. A
somewhat similar proposal, known as "Strategic Budgeting" has been
before the Board as a proposal for a number of years. The Budget Committee believes results based
budgeting (i.e., the Friedman Model) will be a beneficial way to proceed in the
future.
The
Budget Summit proved to be a useful endeavor and resulted in a number of
recommendations, which can be categorized into these four broad categories:
A.
Funding
Should Be More Explicitly Tied to Desired Results
B.
Medicaid/SSDI/SSI
Should Be Re-Tooled as Possible to Achieve Desired Results
C.
The
Planning Committee Should Review Whether the Current Level of Reliance on
Psychiatric Medications is leading to Desired Results.
D.
The
Budget Building Process Should be Re-evaluated.
There are a number of parts to
each of the main recommendations.
The
Budget Committee wholeheartedly supports moving to results based budgeting that
the Trust has been advocating for a number of years, known as the
"Friedman Model." In essence,
the approach is to (1) define what results (also known as outcomes) are
desired, (2) develop measurement(s) for determining how well the system is
doing in "purchasing" desired results, and (3) this data should be
regularly collected, analyzed and acted upon.
In other words, what does the data reveal about effectiveness of
programs? Where are the gaps? What changes
in program funding should be made to achieve desired results? In order to achieve this the Budget Committee
recommends that:
1.
The Planning Committee develop a recommendation
to the full board regarding the desired results; and
2.
The Planning Committee determine/develop
recommendations to the full board regarding what results to measure
3.
Programs should be evaluated and funded based on
recipient results. In other words, goals
and benchmarks should be established and funding based on the extent to which
these are achieved.
4.
Financial incentives should be given providers
for producing desired results.
5.
Grants should be re-tooled to produce desired
results.
6.
Non-traditional and flexible approaches should be
part of the Program and evaluated for achieving desired results along with
traditional approaches.
7.
The
following data should be acquired:
a.
Who
Are the Recipients of the Mental Health Program?
b.
What
services constitute the Mental Health Program?
c.
What
is spent on the total Mental Health Program, including Indian Health Service
spending (Alaska Native Tribal Health Consortium)?
d.
Who
are receiving services?
e.
What
are the results for various populations?
In other words, are there differences in results for different groups of
people, such as Natives or other minorities?
f.
What are the SSDI/SSI Recipient Population
Trends?
g.
What
are the Indian Health Service Population Trends?
h.
What
Are the Results Geographically?
i.
Which Programs are Achieving Desired Results and
Vice Versa?
j.
Why is There Such a Difference in per capita
Medicaid Billing?
The
Medicaid/SSDI/SSI eligibility mechanism has come to dominate Program
financing. Thus, to the extent possible
within federal requirements, this mechanism should be reviewed and adjusted to
achieve desired results. To the maximum
extent possible:
1.
Eligible services should be based on achieving
desired results.
2.
Eligible services should be flexible in order to
allow services to be tailored to what individuals need to achieve desired
results including, if possible, non-traditional approaches.
3.
Disincentives to achieving desired results should
be ferreted out and corrected, where possible.
The
Mental Health System currently relies heavily on psychiatric medications. It is recommended that further research on
how the use of these medications impact desired results should be conducted.
1.
In developing budget
recommendations, the entire Program budget and desired outcomes should be
considered.
2.
While stakeholder input
should always be sought, it should be evaluated in the context of results based
budgeting that considers the entire mental health budget.
3.
The Trust should consider
reviewing its RFR process to determine if it is producing optimal results. Specifically, in addition to taking the
entire Program budget into consideration, the Trust might re-evaluate its
policy of requiring an Exit Strategy to be eligible for Trust funding.
4.
The Board should remember
that its budgetary responsibilities are broader than the Trust's.
5.
Existing and potential
revenue sources should be more seriously pursued, such as:
a.
Federal
Medicaid
b.
Federal
Discretionary
c.
Community
Mental Health Services Block Grants
d.
State
e.
Recipients
f.
Foundations
g.
Trust
Lands - Find Oil and/or Gas on
h.
Partnering
i.
Federally Qualified Health Centers
j.
Others
The
Budget Committee's conclusions arising from the Summit are (1) more data needs
to be developed and regularly evaluated to help steer program funding to
achieve desired results based on data, (2) the precise desired results need to
be determined, based on consumer and community values, and (3) the budget
should be built around purchasing the desired results.
[1] This approach essentially follows what the Alaska Mental Health Trust Authority has been urging for the last few years.
[2] The statute refers to this as Mental Health Trust Authority Authorized Receipts which becomes the acronym MHTAAR.
[3]
[4] A detailed analysis of these expenditures for all of the community mental health centers in the state is attached as Appendix A.
[5] The Trust calls this an "Exit Strategy" meaning that the Trust, as a general matter, is not prepared to continue funding programs indefinitely.